What is the liver and what vital functions does it perform?
The liver is an organ located in the abdominal cavity to the right of the hypochondrium. It is the biggest gland in the human body, and weights around 2.5% of an adult (around 1.5 kg).
Blood detoxification, the synthesis of the most important substances of the blood, glycogenesis, and bilifaction are carried out in the liver. It is also involved in lymphogenesis and the body's metabolizing process.
The most important functions of liver:
- bile production (circa 600 ml a day);
- detoxication;
- detoxication and elimination of excessive agents (hormones, vitamins), of metabolic-waste products;
- hormones level regulation (e.g.: aldosterone, epinephrine (adrenaline), estrogen, insulin);
- participation in digestion;
- conversion of ammonia into urea;
- energetic reserves storage (glycogen);
- carbohydrate metabolism;
- accumulation, storage and delivery of certain vitamins;
- participation in vitamins metabolism (folic acid, А, С, В, D, К, E, РР); conversion of carotene into vitamin A;
- lipid, cholesterol synthesis, lipid metabolism regulation; fat energy restoration;
- synthesis of ferments, hormones which participate in food transformation;
- detoxication of endogenous and exogenous agents (alcohol, toxins, drugs);
- participation in immune functions;
- an important role in blood circulation;
- thermoregulation of body;
- plasma proteins and blood-coagulation factors production.
If the liver stops functioning properly, the problems associated with this may include:
- A disorder of the digestive function of the liver, resulting in a reduced level of bile secretion, can lead to changes to the shape of the organ and an interruption to the normal digestion and absorption of fat in the gastrointestinal tract. This may result in diarrhea and flatulence, and the lack of fat absorption may lead to metabolic alterations, followed by weight loss and even cachexia (muscle loss).
- An interruption to the detoxification (decontaminative) function of the liver cam lead to the blood being impacted by the presence of toxic agents both from outside the body and from those produced by microflora like indole, phenol, or skatole in the large intestine. The presence of these toxins in the blood can produce irreversible damage to the central nervous system including the brain through a process called liver encephalopathy.
- Impacts on the liver's synthetic ability can lead to albumin synthesis inhibition. Albumin is the most important plasma protein. Furthermore, the production of blood-coagulation system proteins can be reduced, eventually resulting in hemostatic derangements that result in even minor injuries producing prolonged bleeding.
Liver disorders are particularly important to address since they quickly become chronic without the necessary treatment, resulting in irreversible damage and ulterior functional abnormality. Despite modern medicine's achievements, some liver disorders do not respond to treatment short of transplantation. It can be the only option in some advanced or severe liver pathologies.
Different diseases and pathologies may serve as indications for liver transplantation:
- Oncological diseases. It should be specified that liver transplantation in case of cancer is indicated when the tumor is located only in liver and the metastases are not defined in other organs.
- Acute liver failure — e.g., as a result of intoxication.
- Severe viral hepatitides (except of hepatitis A).
- Hemochromatosis — a metabolic disturbance, in which iron begins to deposit oneself in liver cells and interferes with its normal functioning.
- Liver cirrhosis in advanced stages, especially if there is a risk of liver coma.
- Wilson’s disease — a disease, in which liver and some other internal organs are affected because of metabolic disturbance.
- Cirrhotic form of cystic fibrosis.
- Congenital malformations, etc.
Absolute contraindications for liver transplantation:
- uncorrectable dysfunctions of vital organs (heart, lungs, central nervous system diseases)
- infection process outside of liver (tuberculosis, HIV-infection, etc.) or any other treatment-resistant systemic or self-limiting infections
- oncological diseases of extrahepatic location
- malformations incompatible with a long-term life
- psychological non-readiness of the patient, his lack of understanding of operation nature, its necessity, risk and estimates
- active alcoholism
Relative contraindications are as follows:
- patient’s age over 60 years old
- liver and bile ducts operation made earlier
- portal vein thrombosis
- cholangiocarcinoma
- active replication of hepatitis B virus
- obesity
- lack of psychological support of the patient on the part of his immediate relatives
What does a liver transplantation represent and what stages does it consist of?
Donor selection stage
A donor should comply with a number of requirements:
- age between 20 and 55 years old;
- blood group compatibility with the recipient’s blood group;
- lack of liver damages and pathologies;
- good general state of health.
Your Journey
A personal assistant supplied by Remed Assistance will welcome you at the airport, accompany you to the hospital and do the necessary translation in order to guarantee a worry-free medical trip experience in Turkey.
Preoperative stage and diagnostics
Currently, a part of an organ, taken from a healthy and living relative of the patient, is being increasingly used. Before the liver transplantation operation, the recipient and the donor undergo an extensive examination that includes as follows:
- Laboratory examination, by means of which the blood group, blood-coagulation factors, biochemical values, presence of hepatitis viruses and human immunodeficiency virus (HIV) is determined.
- Computer tomography, by means of which an image of liver is created, as well as is determined its size and form.
- Doppler ultrasonography, by means of which the state of liver blood vessels is determined.
- Electrocardiography and echocardiography – help to control the state of heart.
- Spirography, by means of which the lung function is determined.
- Pneumonography.
- Psychologist consultation, etc.
In case of identification of any specific health problems, some additional examination methods may be assigned.
Liver transplantation from a living donor, especially from a relevant, is considered to be the most preferred version.
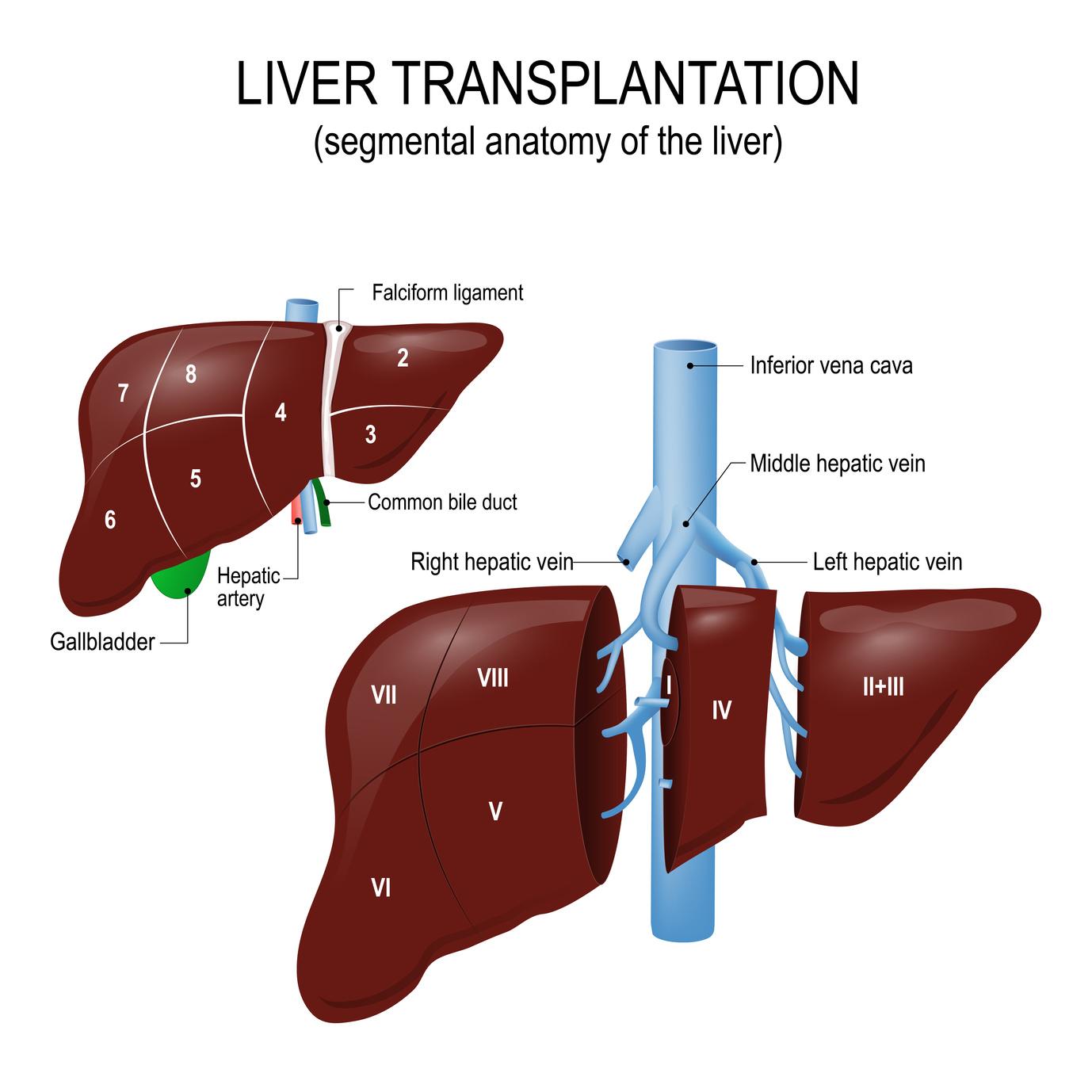
Living-donor transplantation
The liver transplantation operation is very complicated. First of all, the surgeon excises the affected organ together with the fragment of vena cava, blocks the blood vessels that nourish liver. After that, instead of the excised liver there shall be transplanted a part of a donor liver (in case of liver transplantation from a living donor). The surgeon reconnects the blood vessels in order to recover the organ’s blood supply. At the final stage the surgeon recovers the biliary ducts. The gall bladder won’t be transplanted into the patient’s body. A special device is used to remove blood and liquid from liver. Drainage tubes are inserted into the abdominal cavity and are left there sometimes for several days. A tube is inserted into the biliary duct of the patient in order to remove the gall. Very important for the doctors are both the volume of the effused gall and its color. It can be yellow or green. Sometimes the tube is left in the already endured organ for several months.
The whole operation lasts for circa 8 to 12 hours and involves a whole team of specialty doctors.
Postoperative period
After liver transplantation, the patient usually stays for circa 2 to 5 days in the intensive care unit, and averagely in 15 to 20 days, under favorable postoperative period progress, is discharged from the in-patient department. Beginning with the post-transplantation day, the patient starts taking specific drugs – immunosuppressors – lifelong, in order to prevent a donor organ rejection. Every two weeks the patients visit the transplantation center to deliver medical tests and to carry out an abdominal ultrasonography.
Liver transplantation in Turkey
The transplantation issues in Turkey are settled in terms of legislation. The international patients in Turkey are allowed to transplant liver from living relative donor.
The advantages of treatment in Turkey:
You may get recommendations and treatment plan from the medical specialists of the top clinics of Turkey, as well as an alternative opinion regarding the provided or only assigned treatment from the medical specialists of the top clinics.
The advantages of treatment in Turkey are: top-class medical treatment and reasonable prices.
The clinics of Turkey work in accordance with global standards using the best practices of collegues from Europe and USA as well as their own unique experience. Turkey is among the countries that are top requested for treatment.
The citizens of a series of countries are attracted by reasonable prices and a high treatment level in Turkey.
In turkish clinics a psychological comfort and a real kindness of all the medical personnel is guaranteed to the patients.
Departure from airport
You will be accompanied to the airport by a personal assistance. By provided flight authorization and medical report, you will take your flight to home!
Follow up
After your return, Remedhealth.com agents will be available for any future request.
